What Is Chronic Kidney Disease
Chronic Kidney Disease (CKD) is a prevalent but often silent health condition that affects millions worldwide. This progressive ailment occurs when the kidneys gradually lose their ability to function efficiently, impacting overall health.
CKD can silently progress for years, making early detection and management crucial. In this comprehensive article, we delve into the intricate facets of CKD, from its subtle signs and risk factors to its profound effects on various body systems.
We'll explore prevention strategies, management approaches, and how individuals can embrace a kidney-friendly lifestyle to safeguard their health and enhance their quality of life. Use these steps to improving kidney health.
Key Takeaways
- Chronic Kidney Disease (CKD) is a condition characterized by the gradual loss of kidney function over time.
- CKD can be caused by various factors such as diabetes, high blood pressure, and kidney inflammation.
- Prevention strategies like maintaining healthy blood pressure levels and regular check-ups can delay or prevent the onset of CKD.
- CKD progression speed varies among individuals and can be slowed down with proper management and lifestyle changes.
Jump to:
- Key Takeaways
- Understanding Chronic Kidney Disease
- Common Symptoms of Chronic Kidney Disease
- The Impact of Chronic Kidney Disease on Daily Life
- Major Causes Behind Chronic Kidney Disease
- How Chronic Kidney Disease Affects the Body
- Preventive Measures for Chronic Kidney Disease
- Medical Tests for Diagnosing Chronic Kidney Disease
- Treatment Options for Chronic Kidney Disease
- Living With Chronic Kidney Disease
- The Role of Diet in Managing Chronic Kidney Disease
- The Importance of Regular Check-ups in Chronic Kidney Disease Management
- FAQs About CKD
- CKD Is A Complex Condition
Understanding Chronic Kidney Disease
Chronic Kidney Disease is a complex condition that requires a deeper understanding. In this section, we'll begin by defining CKD and exploring its root causes and risk factors. We'll then provide an overview of the stages of CKD (stages of chronic kidney disease), shedding light on the progression of this condition.
By the end, you'll have a clear grasp of what CKD is, what leads to its development, and how it evolves through various stages, empowering you with knowledge to take charge of your kidney health.
For More Recipes and Ideas --->> Get Your Free Meals and Recipes That Are Perfect for Pre-Dialysis Diets, Pre-Dialysis with Diabetes, or Dialysis Diets.
Chronic Kidney Disease Definition
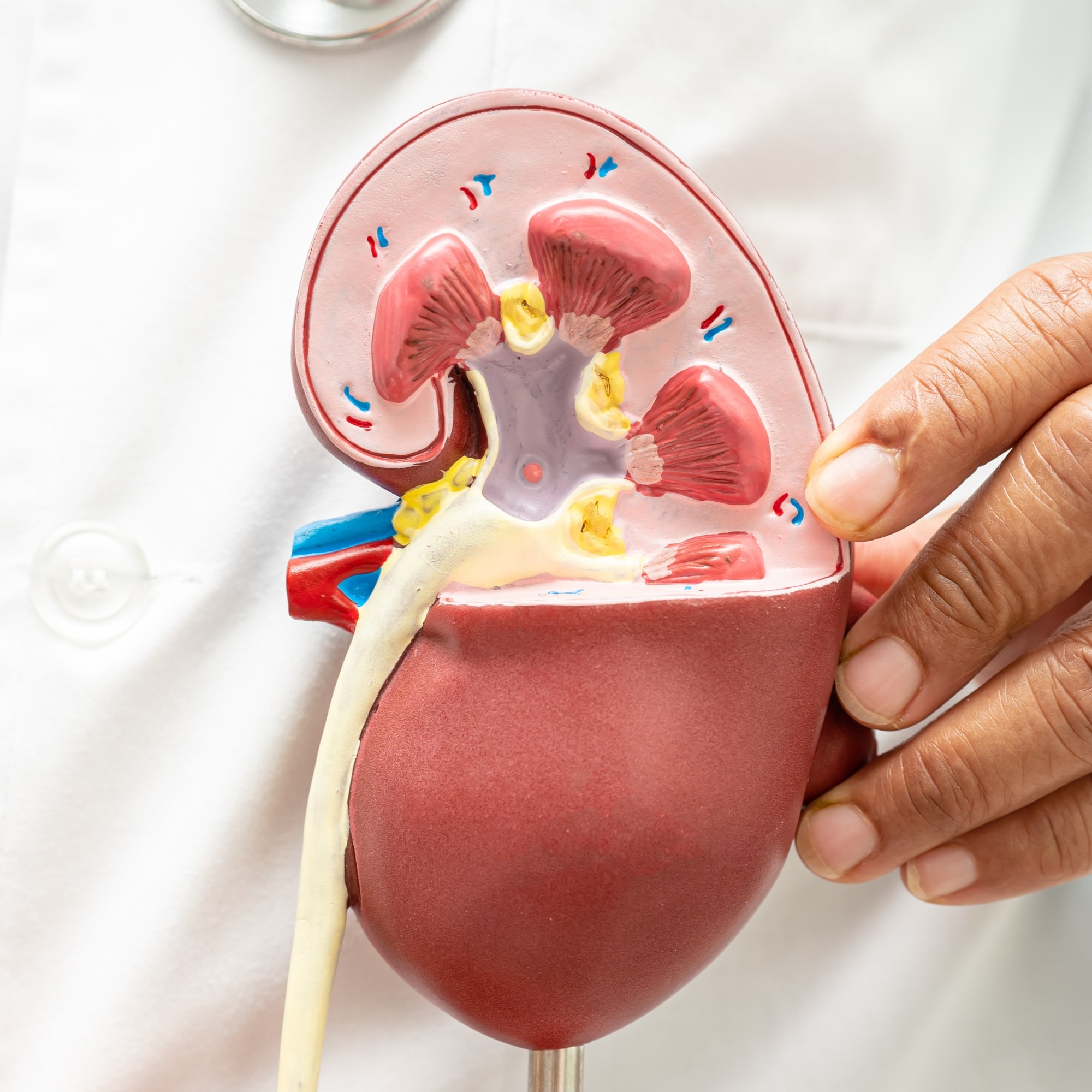
Chronic Kidney Disease is a progressive, long-term medical condition defined by the gradual deterioration of kidney function over an extended period. The kidneys, vital organs responsible for filtering waste products and excess fluids from the bloodstream, become less effective at performing these critical functions in CKD.
This deterioration can lead to an accumulation of toxins in the body, imbalances in fluid and electrolytes, and other complications. CKD often develops silently, with symptoms becoming apparent in advanced stages.
Accurate diagnosis and staging of CKD are determined by measuring the Glomerular Filtration Rate (GFR), a key indicator of kidney function. CKD stages range from mild (Stage 1) to severe (Stage 5), with each stage reflecting a specific level of GFR decline. Early detection and management are essential to slow CKD progression and mitigate its impact on overall health.
Causes and Risk Factors
Chronic Kidney Disease can have multiple causes and risk factors that contribute to its development. Some primary causes include diabetes and high blood pressure (hypertension), which are the most common culprits.
Other contributing factors encompass autoimmune diseases like lupus, recurrent kidney infections, urinary tract obstructions, genetic predispositions, and certain medications that can harm kidney function. Lifestyle choices such as smoking, excessive alcohol consumption, and a diet high in sodium and processed foods can elevate the risk (processed foods and CKD).
Moreover, advancing age plays a role, as kidney function naturally declines with time. Family history of kidney disease and ethnicity can also influence susceptibility. African Americans, Hispanics, and Native American people face a higher risk of CKD.
Recognizing these causes and risk factors is essential for early intervention and prevention efforts to manage and mitigate the progression of CKD.
Kidney Disease Stages
Chronic Kidney Disease is categorized into five stages based on the Glomerular Filtration Rate (GFR), which measures kidney function.
- Stage 1: GFR is greater than or equal to 90 mL/min/1.73 m², indicating kidney damage but still functioning relatively well.
- Stage 2: GFR is between 60 and 89 mL/min/1.73 m², reflecting mild reduction in kidney function.
- Stage 3: GFR is between 30 and 59 mL/min/1.73 m², signifying moderate kidney damage.
- Stage 4: GFR is between 15 and 29 mL/min/1.73 m², indicating severe reduction in kidney function.
- Stage 5: GFR is less than 15 mL/min/1.73 m² or on dialysis, representing end-stage kidney disease (ESKD) where kidneys can no longer effectively filter waste and excess fluids.
These stages help healthcare professionals assess the severity of CKD and guide appropriate management and treatment strategies.
Common Symptoms of Chronic Kidney Disease
Understanding the symptoms of Chronic Kidney Disease is crucial for timely diagnosis and effective management. Symptoms can vary depending on the stage of CKD, and recognizing them early can make a significant difference in your kidney health.
In this section, we will explore the diverse range of symptoms (common symptoms of CKD) that may manifest during different stages of CKD, from subtle early signs to more pronounced late-stage indications. We'll also delve into strategies for symptom management and improving your quality of life while living with CKD.
Identifying Early Stage Symptoms
In the early stages of kidney disease, symptoms may be subtle, making it challenging to detect the condition.
Common symptoms of kidney disease during this phase include increased thirst, frequent urination, especially at night, fatigue, and generalized weakness. Changes in urine color, such as it appearing darker, foamy, or containing blood, may also be noticeable.
Swelling in the ankles and legs, known as edema, can occur due to fluid retention. Additionally, mild hypertension (high blood pressure and kidney disease) can be an early indicator.
These symptoms can vary from person to person, and some individuals may not experience any at all.
Recognizing these signs and seeking medical attention for early diagnosis is crucial, as it allows for timely intervention to slow the progression of kidney disease and prevent complications. Regular kidney function tests can help monitor these symptoms and assess kidney health.
Advanced Kidney Disease Signs
As kidney disease advances, symptoms become more pronounced and can significantly impact one's health and quality of life.
Advanced kidney disease often presents with symptoms such as severe fatigue, persistent nausea, vomiting, and loss of appetite, leading to unintentional weight loss. Edema, or swelling, can extend beyond the legs and feet to affect the face and hands. Excess water accumulation in the lungs can also lead to shortness of breath due to pulmonary congestion.
Patients may experience difficulty concentrating, trouble sleeping, and itchy skin due to the buildup of waste products in the blood. High blood pressure, frequent urination (especially at night), and changes in urine output are common. Additionally, anemia may develop, leading to pale skin and weakness.
Questions about kidney transplant? Advanced kidney disease requires comprehensive medical management and, in many cases, dialysis or kidney transplant to maintain health.
Symptom Management in CKD
Symptom management is a crucial aspect of caring for individuals with Chronic Kidney Disease. Addressing symptoms effectively can greatly improve the patient's health-related quality of life. Managing symptoms (managing renal diet limits) often involves a multi-faceted approach.
- Blood Pressure Control: Controlling high blood pressure is essential in CKD to prevent further kidney damage and reduce symptoms like fatigue and headaches.
- Fluid Balance: Proper fluid management helps avoid edema and maintain electrolyte balance. Restricting fluid intake may be necessary.
- Dietary Modifications: A renal diet can help manage symptoms. Controlling protein, potassium, phosphorus, and sodium intake is vital.
- Medications: Medications can address specific symptoms like anemia (iron supplements and erythropoietin-stimulating agents) and bone health (vitamin D and phosphate binders).
- Pain Relief: Addressing pain, whether from kidney stones or other causes, is essential for patient comfort.
- Symptom-Specific Approaches: Managing symptoms like itching or sleep disturbances with appropriate medications or lifestyle adjustments.
- Emotional Support: CKD can be emotionally taxing, so emotional support and counseling may be beneficial.
A tailored approach, involving healthcare providers, dietitians, and other specialists, is crucial for effective symptom management in CKD.
The Impact of Chronic Kidney Disease on Daily Life
Living with chronic kidney disease often requires you to navigate daily challenges and make significant lifestyle adaptations, particularly regarding your dietary habits.
The emotional toll of CKD is substantial, necessitating a robust support system that understands the intricacies of renal pathology and its physical manifestations.
Moreover, effectively managing alterations in your diet due to nephropathy's metabolic implications becomes pivotal for maintaining optimal health outcomes.
This includes understanding renal-friendly food choices, balancing nutrient intake with dialysis requirements, and potentially implementing conservative management strategies as part of your overall treatment plan (kidney disease treatment diet).
Daily Challenges and Adaptations
Living with Chronic Kidney Disease poses a series of daily challenges that require continuous adaptation and resilience. These challenges span different facets of life, encompassing physical, emotional, and social dimensions.
One significant challenge is adhering to a strict renal diet, which entails limiting protein, potassium, phosphorus, and sodium intake. This can be particularly difficult when dining out or attending social events. CKD patients also grapple with fluid management, as fluid restrictions necessitate constant monitoring of their liquid intake to prevent excess fluid buildup.
Managing a complex regimen of medications (commonly prescribed medications for CKD), including phosphate binders, blood pressure medications, and erythropoietin-stimulating agents, can be overwhelming. CKD patients also face a daily burden of symptoms such as fatigue, itching, and bone pain, which impact their quality of life.
The emotional toll of coping with a chronic illness, including anxiety and depression, adds another layer of daily challenge. For patients on dialysis, frequent treatment sessions demand time and energy. Additionally, CKD may lead to increased healthcare costs and potential job loss, creating financial stress.
To adapt to these challenges, many CKD patients develop a strong support network, seek counseling or mental health support, and actively engage with healthcare providers to effectively manage the disease and enhance their overall quality of life.
Emotional Impact and Support
Chronic Kidney Disease carries a substantial emotional burden for patients. The diagnosis, ongoing symptoms, and potential progression of the disease can lead to feelings of fear, anxiety, depression, and frustration.
It's crucial to address these emotional challenges as they can significantly impact a patient's quality of life and overall well-being.
One of the most effective ways to manage the emotional impact of CKD is through a strong support system. Family, friends, and support groups can provide understanding, empathy, and encouragement. Additionally, seeking professional help from mental health experts or counselors can offer valuable coping strategies and emotional support.
Patients should also prioritize self-care, including stress-reduction techniques like meditation, mindfulness, and relaxation exercises.
Maintaining a positive outlook, setting realistic goals, and staying engaged in activities that bring joy can contribute to better emotional health. Ultimately, acknowledging and addressing the emotional impact of CKD is a crucial aspect of holistic disease management.
Dietary Changes and Management
How much protein in CKD Diets? Dietary changes are a fundamental aspect of managing Chronic Kidney Disease. Patients need to adhere to a renal diet tailored to their specific condition and CKD stage. This typically involves controlling protein intake, limiting phosphorus, potassium, sodium, and fluid, and monitoring calorie intake.
Reducing protein intake helps minimize the burden on the kidneys, as protein metabolism produces waste products that the kidneys must filter.
Monitoring phosphorus, potassium, and sodium levels is essential to prevent electrolyte imbalances, bone problems, and cardiovascular complications. Restricting fluid intake is vital to prevent fluid buildup, which can lead to high blood pressure and edema.
Patients must work closely with dietitians to develop personalized meal plans that meet their nutritional needs while adhering to these dietary restrictions. Proper dietary management plays a crucial role in slowing the progression of CKD and reducing the risk of complications.
Major Causes Behind Chronic Kidney Disease
Understanding the causes of Chronic Kidney Disease is essential for effective prevention and management. While there are various factors that can contribute to CKD, two primary culprits are hypertension (high blood pressure) and diabetes. These conditions exert relentless pressure on the kidneys, gradually impairing their function over time.
Additionally, inherited conditions like polycystic kidney disease and autoimmune conditions such as glomerulonephritis can also lead to CKD.
In this section, we delve into the intricate relationship between these causes and CKD, emphasizing the significance of early detection and intervention to mitigate the risk and impact of this chronic illness.
Diabetes Impact on Kidneys
Diabetes Mellitus is a significant contributor to Chronic Kidney Disease. In diabetes, persistently high blood sugar levels can damage the small blood vessels and filtering units within the kidneys, known as nephrons. This leads to diabetic kidney disease.
This damage progressively impairs the kidneys' ability to filter waste and excess fluids from the bloodstream, leading to a buildup of toxins and fluid retention. Over time, this strain can result in CKD.
Uncontrolled diabetes also prompts inflammation and oxidative stress, further harming kidney tissue. Additionally, diabetes often accompanies high blood pressure, compounding the stress on the kidneys.
To prevent or slow the progression of CKD in diabetic patients, it's crucial to manage blood sugar levels rigorously through medication, diet, and lifestyle adjustments. Regular monitoring and early intervention are paramount in preserving kidney function.
High Blood Pressure Role
Hypertension, or high blood pressure, is a leading cause of Chronic Kidney Disease. The kidneys play a vital role in regulating blood pressure by controlling the volume of blood and the balance of electrolytes in the body.
Prolonged high blood pressure can damage the small blood vessels and nephrons within the kidneys, impairing their ability to filter waste and excess fluids effectively.
As hypertension continues, the kidneys' filtration capacity diminishes, and protein may begin leaking into the urine a sign of kidney damage. The constant pressure also leads to inflammation and oxidative stress within the renal tissue, exacerbating kidney injury.
Managing blood pressure through lifestyle changes and medication is essential for preventing or slowing CKD progression, highlighting the interconnectedness of hypertension and kidney health.
Understanding Inherited Kidney Diseases
Inherited kidney diseases, such as Polycystic Kidney Disease (PKD), can significantly contribute to the development of Chronic Kidney Disease (CKD). PKD is a genetic disorder characterized by the formation of fluid-filled cysts within the kidneys, which gradually replace healthy kidney tissue over time.
These cysts disrupt kidney function by enlarging the kidneys, affecting their ability to filter waste products from the blood. As a result, individuals with PKD often experience high blood pressure (high blood pressure and kidney disease), proteinuria (excess protein in the urine), and impaired kidney function. Over the years, this damage can lead to CKD.
While PKD is a specific example, various inherited kidney diseases can have a similar impact, emphasizing the genetic factors that contribute to CKD development. Early detection and management of these genetic conditions are essential to delay CKD progression and preserve kidney function.
Other Kidney Disease Causes
Chronic Kidney Disease can have various causes beyond diabetes, hypertension, and inherited conditions like Polycystic Kidney Disease. Some notable factors contributing to CKD include:
- Glomerulonephritis: This group of kidney diseases involves inflammation of the glomeruli, the tiny blood vessels in the kidneys responsible for filtering blood. Prolonged or severe cases can lead to CKD.
- Autoimmune Diseases: Conditions like lupus and IgA nephropathy, where the immune system mistakenly attacks the kidneys, can result in CKD.
- Kidney Stones: Recurrent or untreated kidney stones can damage renal tissue and impair kidney function over time.
- Infections: Severe or recurrent kidney infections, such as pyelonephritis, can scar kidney tissue, contributing to CKD.
- Medications: Some drugs, especially if misused or taken in high doses, can be nephrotoxic (harmful to the kidneys) and lead to CKD (commonly prescribed medications for CKD).
- Urinary Tract Obstruction: Blockages in the urinary tract due to conditions like enlarged prostate or kidney tumors can cause CKD by hindering urine flow and damaging the kidneys.
- Congenital Abnormalities: Structural abnormalities in the kidneys or urinary tract present at birth can lead to CKD.
Identifying and managing the underlying cause is crucial to prevent or slow the progression of CKD in these cases. Early detection and intervention remain essential in preserving kidney function.
How Chronic Kidney Disease Affects the Body
Chronic Kidney Disease is a complex condition that profoundly impacts the body, extending well beyond impaired kidney function. While it primarily affects the kidneys, it also wreaks havoc on various organs and systems, leading to a cascade of complications.
One of the most notable and life-threatening consequences of CKD is its profound impact on cardiovascular health, increasing the risk of heart disease and stroke. However, CKD's detrimental effects are not confined to the cardiovascular system; it also influences bone health, metabolism, and immune function.
In this section, we'll explore the multifaceted ways in which CKD can affect the body, with a focus on cardiovascular complications and other organ-related issues.
Cardiovascular Complications
Cardiovascular complications are among the most significant and life-threatening consequences of Chronic Kidney Disease. As kidney function declines, the risk of heart-related problems substantially increases. CKD affects the cardiovascular system through various mechanisms.
Firstly, CKD leads to the accumulation of waste products and excess fluid in the body, causing hypertension (high blood pressure), a major risk factor for heart disease.
Secondly, CKD disrupts mineral and electrolyte balance, such as calcium and phosphorus, which can contribute to vascular calcification, hardening arteries, and increasing the risk of heart attacks and strokes. Additionally, CKD leads to inflammation, oxidative stress, and endothelial dysfunction, further promoting cardiovascular issues.
Managing cardiovascular complications in CKD involves strict blood pressure control, lipid management, and lifestyle modifications. Medications and dialysis may also be necessary. Recognizing the close link between CKD and cardiovascular health is crucial in preventing heart-related complications and improving the overall quality of life for CKD patients.
Effects on Other Organs
Chronic Kidney Disease is a systemic condition that can have far-reaching effects beyond cardiovascular complications. Several other complications can arise as kidney function declines:
- Anemia: CKD often leads to reduced production of red blood cells, causing anemia. Anemia can result in fatigue, weakness, and cognitive impairment.
- Bone Health Issues: CKD affects mineral metabolism, leading to imbalances in calcium and phosphorus. This can cause bone disorders like renal osteodystrophy, increasing the risk of fractures.
- Fluid and Electrolyte Imbalances: CKD can disrupt the balance of fluids and electrolytes in the body, leading to conditions like edema (fluid retention), electrolyte imbalances, and muscle cramps.
- Neurological Complications: CKD can lead to neuropathy, cognitive impairment, and even seizures in severe cases.
- Gastrointestinal Problems: Uremic toxins can affect the digestive system, leading to symptoms like nausea, vomiting, and loss of appetite.
- Immune System Weakness: CKD can impair the immune system's function, making patients more susceptible to infections.
Managing CKD involves addressing these complications through a combination of medications, dietary modifications, and, in later stages, renal replacement therapy like dialysis or kidney transplantation. Regular monitoring and early intervention are crucial in minimizing the impact of these complications on patients' quality of life.
Complications of Kidney Failure
End-Stage Renal Disease (ESRD) or renal failure is the most advanced stage of Chronic Kidney Disease, and it carries several profound complications and implications for affected individuals. One of the most significant implications is the necessity for renal replacement therapy, primarily dialysis or kidney transplantation, as the kidneys have lost their ability to function adequately.
ESRD patients often require frequent and time-consuming dialysis treatments, typically multiple sessions per week. These treatments can disrupt their daily lives, making it challenging to maintain regular employment or engage in usual activities. Additionally, the dietary restrictions and fluid limitations imposed to manage the condition can affect their quality of life.
Cardiovascular complications are prevalent in ESRD, as individuals are at a higher risk of heart disease, hypertension, and strokes due to fluid imbalances, electrolyte abnormalities, and the accumulation of waste products in the bloodstream. In fact, cardiovascular events are the leading cause of death in people with kidney disease.
Severe anemia is common among ESRD patients, leading to fatigue and reduced overall well-being. Many require regular injections of erythropoietin to manage this condition.
ESRD can also affect bone health, potentially causing bone pain and an increased risk of fractures. Mental health concerns such as depression and anxiety often accompany the diagnosis due to the emotional and psychological challenges associated with the disease, including the burden of regular treatments and the need for dietary restrictions.
For many individuals with ESRD, kidney transplantation offers a better quality of life compared to long-term dialysis. However, access to suitable donor organs can be limited, and transplant recipients must commit to lifelong immunosuppressive medications to prevent organ rejection.
The financial and social impact of ESRD is substantial, affecting not only patients but also their families. The cost of ongoing treatments, medications, and potential lifestyle adjustments can be a significant burden.
Preventive Measures for Chronic Kidney Disease
Preventing Chronic Kidney Disease is a paramount goal in healthcare, given its significant impact on individuals' well-being and the healthcare system. This section delves into proactive measures to prevent CKD, focusing on identifying risk factors, adopting a healthy lifestyle, and emphasizing the importance of routine check-ups.
By understanding and managing risk factors such as hypertension, diabetes, and obesity, individuals can take proactive steps to reduce their vulnerability to CKD. Lifestyle choices, including maintaining a balanced diet, staying physically active, and avoiding harmful substances, play a pivotal role in kidney health.
Regular medical check-ups are crucial for early detection and intervention, enabling healthcare providers to address potential issues promptly and optimize kidney health.
Risk Factors Identification
Identifying risk factors for Chronic Kidney Disease is vital for early prevention and intervention. Common risk factors include hypertension (high blood pressure), diabetes, a family history of kidney disease, and a history of recurrent kidney infections. By recognizing these factors, individuals can take proactive steps to minimize their risk.
Hypertension and diabetes are two major contributors to CKD. Managing blood pressure through lifestyle changes and medications, as well as controlling blood sugar levels, can significantly reduce the risk of kidney damage. Additionally, being aware of family history prompts increased vigilance and regular screenings.
A history of kidney infections underscores the importance of promptly treating urinary tract infections to prevent kidney damage. Other risk factors, such as obesity and smoking, can also impact kidney health.
Routine check-ups with healthcare providers can help assess and monitor these risk factors. Early detection and management are key to preventing or slowing the progression of CKD, preserving kidney function, and enhancing overall health.
Healthy Lifestyle Adoption
Maintaining a healthy lifestyle plays a pivotal role in preventing Chronic Kidney Disease. It starts with identifying and addressing potential risk factors. Understanding your personal risk, whether it's due to diabetes, hypertension, a family history of kidney disease, or other factors, empowers you to take proactive measures.
A key aspect of prevention is adopting a kidney-friendly diet. This includes reducing sodium intake, limiting processed and high-sugar foods, and monitoring phosphorus and potassium levels, especially if you have underlying kidney risk factors. Staying adequately hydrated without overloading on fluids is equally important.
Controlling blood pressure and blood sugar levels is crucial. Regular monitoring, medication adherence, and lifestyle adjustments can help manage these risk factors effectively. Incorporating physical activity into your routine not only aids in weight management but also contributes to overall health.
Avoiding smoking and excessive alcohol consumption can protect kidney function. Additionally, being mindful of over-the-counter medications, especially non-steroidal anti-inflammatory drugs (NSAIDs), and consulting a healthcare provider before their regular use is essential.
Consider this table showcasing key areas to focus on:
| Category | Why It Matters | What You Can Do |
| Exercise Benefits | Regular physical activity aids renal function. | Engage in moderate exercise regularly. |
| Stress Management | High stress can worsen CKD symptoms. | Adopt relaxation techniques like meditation. |
| Sleep Importance | Good sleep promotes overall health, vital for CKD patients. | Maintain regular sleep schedule. |
| Alcohol Consumption & Smoking Effects | Both habits exacerbate CKD damage. | Limit alcohol intake; quit smoking entirely if possible. |

Regular Check-ups Importance
Regular check-ups are a cornerstone of Chronic Kidney Disease prevention. These evaluations offer a crucial opportunity to monitor your kidney health, identify risk factors, and detect early signs of kidney dysfunction. During these check-ups, healthcare professionals assess your blood pressure, blood sugar levels, and conduct urine tests and blood tests to detect abnormalities like proteinuria.
Early detection and intervention are vital in preventing CKD progression. If risk factors are identified, such as diabetes or hypertension, healthcare providers can work with you to manage these conditions effectively, reducing their impact on kidney health. Routine check-ups also enable adjustments to medications or lifestyle changes as needed.
Moreover, monitoring kidney function through estimated glomerular filtration rate (eGFR) assessments and serum creatinine levels helps in recognizing any decline in kidney function at an early stage. By addressing issues promptly and adopting preventive measures, the risk of CKD development or progression can be significantly reduced, ultimately safeguarding kidney health.
Medical Tests for Diagnosing Chronic Kidney Disease
This section delves into the essential tests used for diagnosing and monitoring Chronic Kidney Disease. Accurate diagnosis and continuous monitoring are vital in managing CKD effectively, as they provide critical insights into kidney function and overall health. From estimated glomerular filtration rate calculations to urine albumin tests, understanding these diagnostic tools is crucial for healthcare providers and individuals alike.
These tests enable the timely identification of CKD, assessment of its stage, and monitoring of disease progression. By exploring these diagnostic measures, you can gain a comprehensive understanding of how CKD is diagnosed and tracked, empowering you to take proactive steps in managing your kidney health.
Kidney Function Testing Methods
Various tests are employed to measure kidney function and assess the glomerular filtration rate (GFR), a key indicator of kidney health. These tests play a crucial role in diagnosing and monitoring Chronic Kidney Disease. Here is a table summarizing some common kidney function tests (chronic kidney disease laboratory tests) and their purposes:
| Test | Purpose |
| Serum Creatinine | Measures waste product buildup in the blood. Elevated levels can indicate reduced kidney function. |
| Blood Urea Nitrogen (BUN) | Assesses kidney and liver function. Elevated levels may suggest impaired kidney function. |
| Estimated GFR (eGFR) | Calculates GFR based on serum creatinine levels. Used to stage CKD and monitor progression. |
| Urinalysis | Analyzes urine for protein, blood, and other abnormalities. Proteinuria and hematuria may indicate kidney damage. |
| Urine Albumin-to-Creatinine Ratio (ACR) | Measures the level of albumin in urine. Elevated levels can indicate kidney damage, especially in diabetes. |
| Serum Cystatin C | A more precise GFR estimator, useful when creatinine results may not be reliable, particularly in older adults. |
These tests help healthcare providers evaluate kidney function, identify abnormalities, and determine the stage of CKD, enabling timely interventions to manage and slow disease progression. Regular monitoring of these markers is essential for individuals at risk of or diagnosed with CKD to maintain kidney health.
Other Tests
In addition to blood and urine tests, healthcare providers may use kidney biopsy and imaging studies to diagnose and evaluate Chronic Kidney Disease (CKD).
Kidney Biopsy: This invasive procedure involves taking a small sample of kidney tissue for examination under a microscope. It helps identify the cause of kidney damage and determine the extent of damage, such as scarring or inflammation. Biopsies are often performed when the cause of CKD is unclear or to guide treatment decisions.
Imaging Tests: Imaging techniques like ultrasound, CT scans, or MRIs may be used to visualize the kidneys' structure and identify any structural abnormalities, such as cysts, tumors, or obstructions. These tests can help diagnose conditions contributing to CKD and assess kidney size and shape.
These diagnostic tools, when combined with blood and urine tests, provide a comprehensive picture of kidney health, allowing for an accurate diagnosis and tailored treatment plans for individuals with CKD.
Follow-up and Monitoring
Regular follow-up and monitoring of lab results with a physician or nephrologist are crucial steps in preventing Chronic Kidney Disease or slowing its progression. These check-ups serve several essential purposes.
First, they enable the early detection of any changes in kidney function (early stage kidney disease). Even minor abnormalities in blood or urine tests can be indicative of kidney dysfunction, and detecting issues at an early stage allows for prompt intervention and lifestyle modifications.
Second, monitoring helps healthcare providers adjust treatment plans as needed. For individuals with risk factors like diabetes or hypertension, close monitoring ensures that blood pressure and blood sugar levels are well-controlled, reducing the risk of kidney damage.
Third, regular check-ups are vital for preventing the progression of established CKD. They help track the rate of kidney function decline, and physicians can make recommendations for dietary changes, medications, and lifestyle modifications to slow down the progression of the disease.
Lastly, these follow-ups allow for individualized care plans tailored to each patient's unique needs. In summary, ongoing monitoring with healthcare professionals is essential for preventing CKD, managing risk factors, and optimizing kidney health for those already diagnosed with the condition.
Treatment Options for Chronic Kidney Disease
CKD treatment options span various stages of the disease. Initially, lifestyle changes and medications are key. Lifestyle modifications include adopting a kidney-friendly diet, managing blood pressure, and addressing underlying conditions like diabetes. Medications help manage complications such as anemia or mineral imbalances.
How to prevent end stage renal disease. As CKD progresses, especially in End-Stage Renal Disease (ESRD), more intensive interventions are needed. Dialysis, involving hemodialysis or peritoneal dialysis, becomes essential to filter waste and excess fluids from the blood when the kidneys falter. In select cases, kidney transplantation offers the prospect of an improved quality of life and better long-term outcomes.
This section explores these diverse treatment modalities, from lifestyle adjustments to medical interventions, for managing CKD.
Medication Management
CKD patients may require a range of medications to manage their condition and associated complications. Here are some common medications:
- Angiotensin-Converting Enzyme (ACE) Inhibitors and Angiotensin II Receptor Blockers (ARBs): These drugs help control blood pressure and reduce proteinuria, slowing kidney damage.
- Diuretics: Diuretics like furosemide help manage fluid retention and swelling often seen in CKD.
- Erythropoiesis-Stimulating Agents (ESAs): These stimulate red blood cell production to combat anemia common in CKD.
- Phosphate Binders: These help regulate phosphorus levels in the blood to prevent bone and heart problems.
- Statins: To manage high cholesterol levels, reducing cardiovascular disease risk.
- Iron Supplements: Often needed to treat anemia.
- Calcium Supplements: To counteract low calcium levels in advanced CKD.
- Vitamin D Supplements: To manage bone health.
Medications are prescribed based on the patient's specific needs, stage of CKD, and individual health factors. Regular monitoring and adjustments are crucial to ensure the best outcomes. Always consult a healthcare professional for personalized guidance and medication management.
Dialysis and Kidney Transplants
For individuals with End-Stage Renal Disease (ESRD), two primary treatment options are dialysis and kidney transplant. The choice between them depends on various factors:
Dialysis: Dialysis is a life-saving treatment that mechanically filters waste and excess fluid from the blood when the kidneys can no longer perform this function.
There are two types: hemodialysis (using a machine) and peritoneal dialysis (using the abdominal lining). Dialysis is effective in managing ESRD and improving symptoms, but it's a lifelong commitment and may require frequent sessions.
Kidney Transplant: A kidney transplant involves surgically replacing a failed kidney with a healthy one from a living or deceased donor. Transplants offer a better quality of life, fewer dietary restrictions, and less time spent on treatment compared to dialysis. However, finding a suitable donor and the risk of organ rejection are challenges.
The choice between dialysis and transplant depends on individual circumstances, including overall health, age, lifestyle, and the availability of a suitable donor. Some patients may initially opt for dialysis while awaiting a transplant. Ultimately, a nephrologist will help determine the best treatment approach for ESRD management.
Lifestyle Modifications for CKD Management
Lifestyle modifications are integral to Chronic Kidney Disease management, significantly impacting patients' overall well-being and slowing disease progression.
Dietary Adjustments: A renal diet, individualized to each patient's stage and specific needs, helps regulate protein, sodium, potassium, and phosphorus intake. Monitoring fluid intake is essential to prevent fluid overload.
Physical Activity: Regular exercise improves cardiovascular health, manages weight, and helps control blood pressure. It can also alleviate symptoms like fatigue.
Medication Adherence: Taking prescribed medications as directed, especially for blood pressure and blood sugar control, is vital in CKD management.
Avoiding Nephrotoxic Substances: Steering clear of tobacco, recreational drugs, and excessive alcohol is crucial, as these substances can harm kidney function.
Blood Pressure and Diabetes Management: Lifestyle changes, including reducing salt intake and managing stress, contribute to maintaining optimal blood pressure and blood sugar levels.
Regular Monitoring: Routine check-ups with healthcare providers enable the timely adjustment of medications and early detection of complications.
Collectively, these modifications enhance patients' quality of life, slow disease progression, and reduce the risk of complications, making them fundamental aspects of CKD management.
Living With Chronic Kidney Disease
As someone living with chronic kidney disease (CKD), you're likely grappling with significant lifestyle adaptations. These adaptations range from modifications in your daily activities to drastic dietary changes.
It's essential to understand how nephron damage necessitates a renal-friendly diet. This diet limits proteins, phosphorus, and potassium that could exacerbate your condition.
Furthermore, managing the emotional impact of CKD is crucial. Feelings of stress or depression can not only affect your quality of life but also influence disease progression and treatment outcomes.
Daily Life Adaptations
Once diagnosed with Chronic Kidney Disease, daily living routines must undergo significant adaptations to effectively manage the condition. These changes encompass various aspects of life, including dietary modifications, careful monitoring of fluid intake, adherence to prescribed medications, and a commitment to regular medical check-ups.
Dietary adjustments are a cornerstone of CKD management, with individuals often following a renal diet. This involves meticulous control of protein, sodium, potassium, and phosphorus intake, necessitating careful meal planning and portion size awareness. Learn how to reduce sodium intake on a renal diet.
Monitoring fluid intake becomes crucial, as CKD patients may need to limit it to prevent complications like fluid overload, swelling, and high blood pressure.
Strict adherence to prescribed medications, particularly those for blood pressure and blood sugar control, is essential for maintaining overall health and kidney function.
Regular medical check-ups with healthcare providers are indispensable for monitoring kidney function, making necessary medication adjustments, and detecting potential complications early. These adaptations, though challenging, are vital for maintaining kidney health, slowing disease progression, and enhancing the overall quality of life for individuals with CKD.
Emotional Impact Management
The emotional impact of Chronic Kidney Disease can be profound, affecting one's mental well-being and quality of life. The diagnosis often brings feelings of fear, anxiety, depression, and frustration. Coping with the physical limitations and lifestyle changes required can be emotionally challenging.
Managing the emotional impact of CKD involves several strategies. Firstly, open communication with healthcare providers and seeking psychological support, such as counseling or therapy, can provide a safe space to express emotions and develop coping strategies.
Support from family and friends is invaluable, and joining support groups or online communities with fellow CKD patients can provide a sense of belonging and shared experiences.
Practicing stress-reduction techniques like mindfulness, meditation, or yoga can help alleviate anxiety. Additionally, maintaining a positive outlook, setting achievable goals, and focusing on what can be controlled rather than dwelling on the disease's limitations can contribute to emotional well-being. Overall, addressing the emotional impact of CKD is a vital aspect of holistic disease management.
The Role of Diet in Managing Chronic Kidney Disease
The renal diet plays a pivotal role in managing Chronic Kidney Disease (CKD). This specialized dietary approach is designed to alleviate stress on the kidneys, slow disease progression, and maintain overall health.
Understanding how dietary adjustments impact CKD management is crucial for patients and caregivers. It involves precise control of protein, potassium, phosphorus, sodium, and fluid intake. These adjustments can help manage symptoms, regulate blood pressure, and delay the need for dialysis.
In this section, we explore the intricacies of the renal diet, offering insights into what to eat and what to avoid, empowering individuals with CKD to make informed choices that support their kidney health and overall well-being.
Dietary Adjustments for Patients
Dietary adjustments for individuals on a renal diet are essential to slow the progression of Chronic Kidney Disease and manage associated complications. These adjustments typically include:
- Protein Restriction: Reducing protein intake helps lessen the burden on the kidneys. High-quality protein sources with essential amino acids are preferred. How much protein in CKD Diets?!
- Potassium Management: Regulating potassium intake is crucial, as high levels can affect heart rhythm. Patients are advised to limit potassium-rich foods like bananas, oranges, and potatoes.
- Phosphorus Control: Restricting phosphorus is vital to prevent bone and cardiovascular issues. Patients must avoid high-phosphorus foods like dairy products, nuts, and certain beans.
- Sodium Limitation: Reducing sodium intake helps control blood pressure and fluid retention. Processed foods, canned goods, and excessive salt usage should be minimized.
- Fluid Management: Monitoring fluid intake is essential to avoid fluid overload, which can strain the heart and lungs.
- Individualization: Dietary plans should be personalized based on CKD stage, comorbidities, and nutritional needs. Regular monitoring and consultation with a dietitian are crucial to maintaining a balanced renal diet while meeting dietary restrictions.
Food Restrictions in CKD
In Chronic Kidney Disease, certain foods should be avoided or limited to prevent the accumulation of harmful waste products and manage associated complications. These include:
- High-Protein Foods: Excessive protein intake can strain the kidneys. Red meat, processed meats, and high-protein dairy products should be limited.
- High-Potassium Foods: Elevated potassium levels can disrupt heart function. Foods like bananas, oranges, tomatoes, and potatoes should be consumed in moderation (leaching potatoes).
- High-Phosphorus Foods: Phosphorus buildup can lead to bone and cardiovascular problems. Avoid or limit dairy, nuts, seeds, and processed foods with phosphorus additives.
- High-Sodium Foods: Excess sodium can worsen blood pressure and fluid retention. Processed foods, canned soups, and restaurant/fast food items are often high in sodium.
- High-Sugar Foods: High sugar intake can contribute to diabetes, a common cause of CKD. Reducing sugary snacks and drinks is advisable.
- Excessive Fluids: Fluid intake should be regulated to avoid fluid overload and swelling.
Individual dietary recommendations may vary based on CKD stage and individual health needs, so consulting with a healthcare provider or dietitian is essential for personalized guidance.
Impact of Healthy Eating
Embracing a kidney-friendly diet (kidney friendly diet for diabetics) is crucial when managing Chronic Kidney Disease as it offers numerous benefits.
Firstly, it can significantly slow down the progression of CKD, helping to preserve kidney function for a longer period. This diet also aids in blood pressure control, which is essential for reducing the risk of complications. Monitoring fluid intake is another key aspect, as it prevents fluid buildup and swelling, a common issue in CKD.
Additionally, a well-structured kidney-friendly diet can alleviate various symptoms associated with CKD, such as nausea, fatigue, and loss of appetite. It also plays a vital role in reducing the accumulation of waste products and toxins in the blood, which can further deteriorate kidney function.
Furthermore, this diet often aligns with heart-healthy eating practices, benefiting overall cardiovascular health. While making dietary adjustments can be challenging, especially when certain foods need to be restricted, the guidance of a registered dietitian experienced in kidney nutrition can provide personalized strategies to make the transition smoother and more sustainable.
The Importance of Regular Check-ups in Chronic Kidney Disease Management
Routine check-ups are the cornerstone of effective Chronic Kidney Disease management. These regular visits to healthcare providers play a pivotal role in assessing kidney function, monitoring disease progression, and tailoring treatment plans.
In this section, we delve into the importance of these check-ups, emphasizing how they can help detect issues early, prevent complications, and guide lifestyle and medication adjustments.
Whether you're living with CKD or are at risk, understanding the significance of these regular appointments and what to expect during them is essential for proactive kidney health management.
Check-ups for Early Detection
Regular check-ups are instrumental in the early detection of Chronic Kidney Disease. These routine visits to your healthcare provider serve as a proactive approach to identify kidney problems at their nascent stages.
Detecting CKD early provides a crucial window of opportunity for interventions that can slow or even halt its progression, preventing it from reaching advanced and potentially irreversible stages.
During these check-ups, various tests, including blood pressure monitoring, urine analysis, and glomerular filtration rate (GFR) assessment, are performed to assess kidney function and overall health.
By identifying CKD in its early phases, healthcare professionals can tailor treatment plans, implement lifestyle changes, and prescribe medications that enhance the chances of preserving kidney function and improving long-term outcomes.
Monitoring Kidney Function Regularly
Regular monitoring of kidney function is critically important for individuals with Chronic Kidney Disease. CKD is a progressive condition that can worsen over time, and its early stages may be asymptomatic.
Monitoring involves frequent check-ups with healthcare providers to assess kidney health, including tests to measure glomerular filtration rate and check for markers of kidney damage in blood and urine.
This ongoing monitoring serves several crucial purposes. First, it allows healthcare professionals to track the progression of CKD, adjusting treatment plans accordingly. Second, it helps identify any complications or comorbidities associated with CKD, such as hypertension or anemia (anemia and dialysis), which can then be managed promptly.
Finally, regular monitoring empowers patients to actively engage in their care and make necessary lifestyle adjustments to slow disease progression, improve overall health, and ultimately enhance their quality of life.
Role of a Nephrologist
A nephrologist plays a pivotal role in managing Chronic Kidney Disease. These specialized kidney doctors are experts in diagnosing, treating, and monitoring kidney-related conditions.
When you have CKD, a nephrologist becomes your primary healthcare partner in ensuring the best possible outcomes.
Their role includes:
- Diagnosis and staging: Nephrologists accurately diagnose CKD, determine its stage based on glomerular filtration rate (GFR), and identify underlying causes.
- Treatment planning: They develop a personalized treatment plan, which may include medication management, lifestyle modifications, and dietary guidance.
- Monitoring: Nephrologists closely monitor kidney function through regular check-ups, adjusting treatment as needed to slow disease progression.
- Complications management: They address complications like hypertension and anemia that often accompany CKD.
- Education: Nephrologists educate patients about CKD, empowering them to actively participate in their care.
Their expertise is invaluable in helping patients navigate CKD, manage symptoms, and make informed decisions to improve their kidney health.
FAQs About CKD
Yes, there can be a genetic predisposition to Chronic Kidney Disease. Some kidney conditions, such as polycystic kidney disease (PKD) and Alport syndrome, are hereditary and can be passed down through generations.
Additionally, certain genetic factors may increase the risk of developing CKD, especially when combined with other risk factors like high blood pressure or diabetes.
Genetic testing and family history assessment can help identify individuals at higher risk, allowing for early monitoring and intervention to mitigate the progression of CKD.
The life expectancy of someone diagnosed with Chronic Kidney Disease varies widely and depends on several factors, including the stage of CKD, the underlying cause, overall health, and the effectiveness of management. In the early stages, with proper care and lifestyle modifications, individuals may have a relatively normal lifespan.
However, in advanced stages, CKD can lead to End-Stage Renal Disease, requiring dialysis or transplantation, which can impact life expectancy. Timely diagnosis, adherence to treatment, and addressing underlying causes like diabetes or hypertension can help improve outcomes and extend life expectancy. It's crucial to consult a healthcare professional for personalized guidance.
Chronic Kidney Disease cannot typically be fully reversed once it has progressed, but early detection and appropriate management can help slow down its progression and preserve kidney function.
While it may not be possible to completely reverse the damage, timely medical interventions, lifestyle changes, and medications can significantly improve a person's quality of life and delay the need for more advanced treatments like dialysis or kidney transplantation.
Regular monitoring and adherence to a kidney-friendly lifestyle are crucial for managing CKD effectively.
Chronic Kidney Disease can have significant implications for pregnancy and fertility. Advanced CKD may lead to fertility issues, as hormonal imbalances can disrupt menstrual cycles. Pregnancy in women with CKD is considered high-risk, as it can lead to complications for both the mother and the baby.
It increases the risk of preeclampsia, preterm birth, and low birth weight. CKD can also worsen during pregnancy. Therefore, individuals with CKD planning to conceive should consult with a healthcare provider for careful management and monitoring to optimize their chances of a healthy pregnancy and baby.
CKD Is A Complex Condition
Chronic Kidney Disease is a progressive condition influenced by factors like diabetes, high blood pressure, and kidney inflammation. However, the good news is that prevention is possible through measures like blood pressure control and routine check-ups, which can delay or avert CKD's onset.
It's important to recognize that CKD progression varies from person to person, and its advance can be significantly slowed through diligent management and adopting a healthy lifestyle. By understanding the risks, taking proactive steps, and embracing the importance of timely intervention, individuals can better safeguard their kidney health and enjoy a higher quality of life.